These positions can help you relax and breathe easier.
Leaning on a table
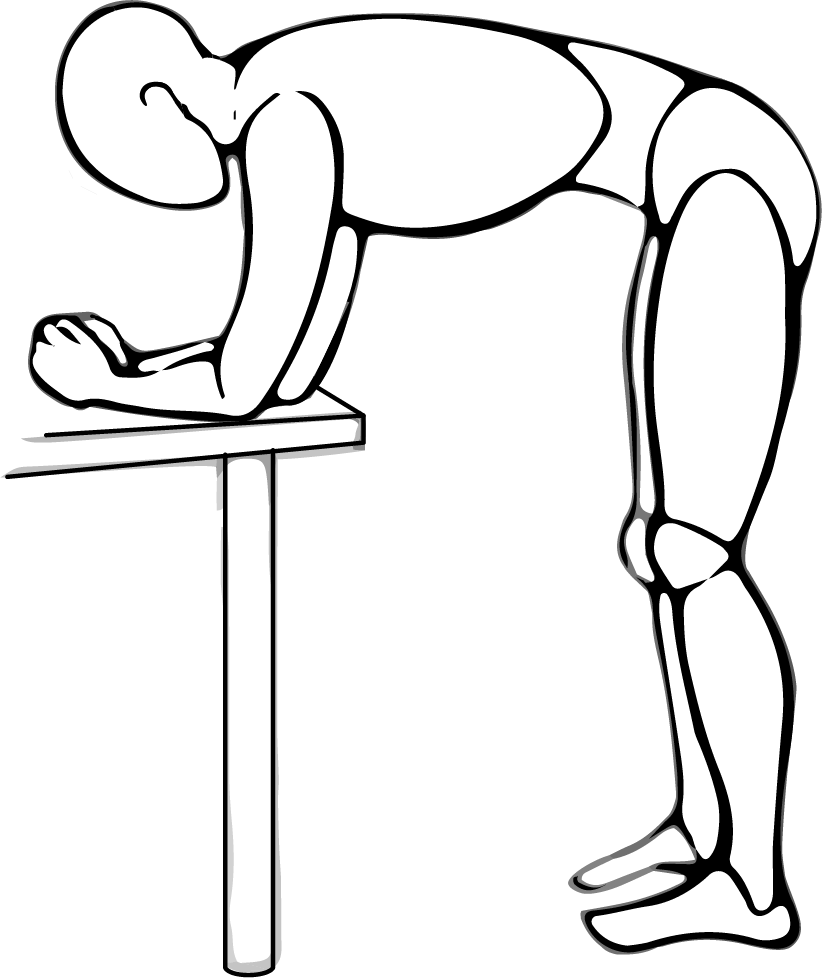
Stand and lean forward on a table.
Rest your elbows and lower arms on the table.
Spread your arms wide apart.
Keep your back straight.
Lying on pillows in bed

Stack pillows on your bed to make a slope.
You can stack them on top of your mattress or under your mattress.
Lie down on your side.
Make sure your whole side is supported.
Resting on pillows stacked on a table
Sit on a chair in front of a table, keeping your feet on the floor.
Stack pillows on the table to the height of your chest.
Lean forward from your hips, keeping your back straight.
Rest your head, upper chest and shoulders on the pillows.
Your arms should be relaxed and resting on the table.
Leaning against a wall

Lean the lower half of your back against a wall.
Place your feet about 30 cm (12 inches) from the wall.
Relax your shoulders.
Your arms should be hanging loosely by your side.
Sitting on a chair

Sit on a chair, keeping your feet on the floor.
Lean forward, keeping your back straight.
Rest your forearms on your thighs.
Relax your wrists.

