Updated 2023 March
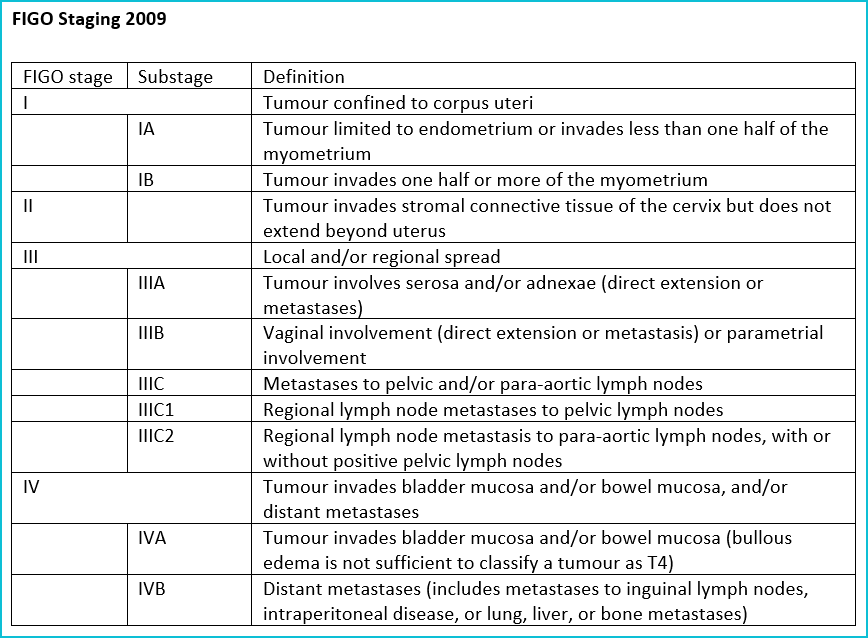
NB: Omentum or peritoneal disease = Stage IVB
- Endometrial Cancer Classification
Endometrial cancer (EC) is the most common gynecologic malignancy in Canada, and the incidence and mortality continue to rise globally. Historically, Bokhman described two types of EC based on distinct epidemiological factors and clinical behaviour. Type I EC corresponded to the estrogen dependent low-grade endometrioid adenocarcinomas that typically had a favourable prognosis. Type II EC corresponded to the estrogen independent non-endometrioid carcinomas which typically showed more aggressive disease with a poor prognosis. The main problem with this historic classification system was the difficulty in applying it to diagnostic practice, as grade and histotype assignment in EC have both been shown to be poorly reproducible, even amongst expert pathologists. This inconsistency can mean that depending on who interprets a pathology specimen, an individual patient could be assigned to a different risk group and receive different treatment recommendations. Inconsistency in diagnosis has also meant that biologically diverse tumours are grouped together in clinical trials making interpretation of treatment efficacy challenging or impossible.
To address these problems, in 2013 The Cancer Genome Atlas (TCGA) Project applied in depth genomic, proteomic, and transcriptomic methodologies to a cohort of ECs identifying four molecular subtypes with distinct prognoses; POLE ultramutated, microsatellite instability (MSI) hypermutated, copy-number low and copy-number high (1). Following this discovery, two research teams independently worked to develop and validate a pragmatic EC classification system that recapitulated the survival curves of the TCGA and identified molecular subtypes through clinically applicable, comparably low cost and easy to interpret assays (2-6). This uses a combination of focused next generation sequencing (NGS) for the detection of pathogenic POLE mutations, and immunohistochemistry (IHC) to assess mismatch repair proteins and p53 status, to assign EC to one of four groups: POLEmut, mismatch repair deficient (MMRd), p53abn and NSMP (no specific molecular profile) (Table below and See MOLECULAR TESTING section for [A1] further details on these molecular tests).
| Molecular Subtypes of Endometrial Cancer | Frequency (%) |
| POLEmut | ~5 |
| Mismatch Repair Deficient (MMRd) | ~30 |
| No Specific Molecular Profile (NSMP) | ~50 |
| p53 abnormal | ~15 |
Unlike histopathological evaluation, the molecular subtyping of EC offers an objective and reproducible classification system that has been shown to have strong prognostic value and therapeutic implications. In Dec 2020, the World Health Organization (WHO) recommended the integration of molecular parameters in to standard pathology reporting where available and molecular classification is also now incorporated in many Societal guidelines (NCCN, ESGO/ESTRO/ESP).
NB MMR and p53 IHC are available in any pathology laboratory and is now considered standard of care for all ECs in BC. POLE testing has been approved in BC since May 2022. Testing in the current funding scheme is being paid for, for patients in whom information on POLE status would impact adjuvant treatment decisions (see POLE testing section below).
- Getz G, Gabriel SB, Cibulskis K, et al. Integrated genomic characterization of endometrial carcinoma. Nature 2013; 497: 67–73.
- Talhouk A, McConechy MK, Leung S, et al. A clinically applicable molecular-based classification for endometrial cancers. Br J Cancer 2015; 113: 299–310.
- Talhouk A, McConechy MK, Leung S, et al. Confirmation of ProMisE: A simple, genomics-based clinical classifier for endometrial cancer. Cancer 2017; 123: 802–813.
- Kommoss S, McConechy MK, Kommoss F, et al. Final validation of the ProMisE molecular classifier for endometrial carcinoma in a large population-based case series. Ann Oncol 2018; 29: 1180–1188.
- Stelloo E, Nout RA, Osse EM, et al. Improved risk assessment by integrating molecular and clinicopathological factors in early-stage endometrial cancer-combined analysis of the PORTEC cohorts. Clin Cancer Res 2016; 22: 4215–4224.
- Stelloo E, Bosse T, Nout RA, et al. Refining prognosis and identifying targetable pathways for high-risk endometrial cancer; A TransPORTEC initiative. Mod Pathol 2015; 28: 836–844.
