Revised 16 October 2012
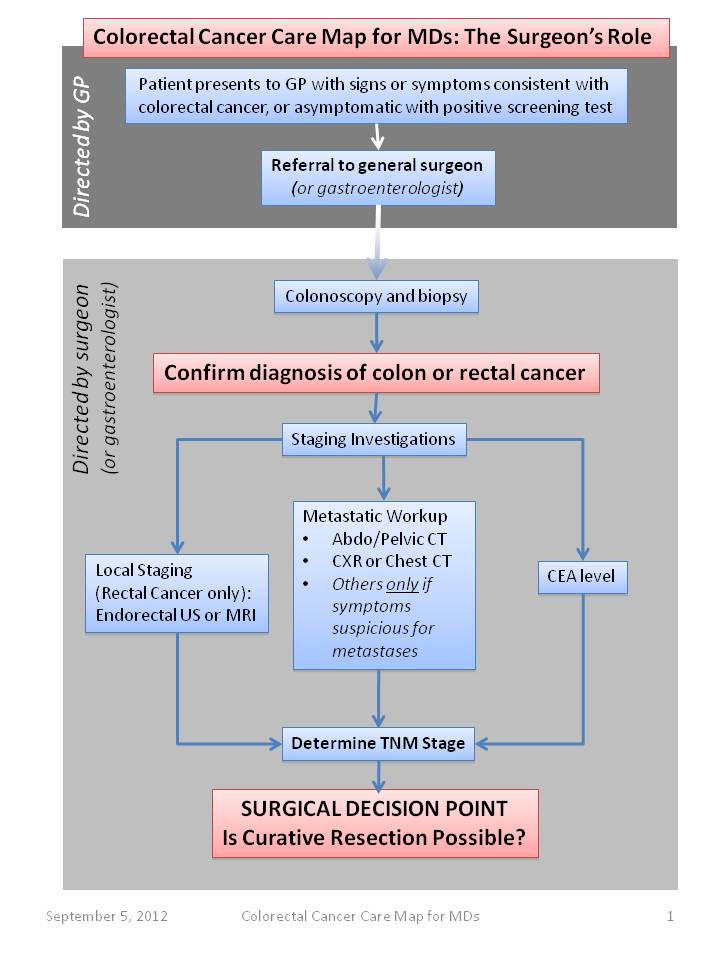
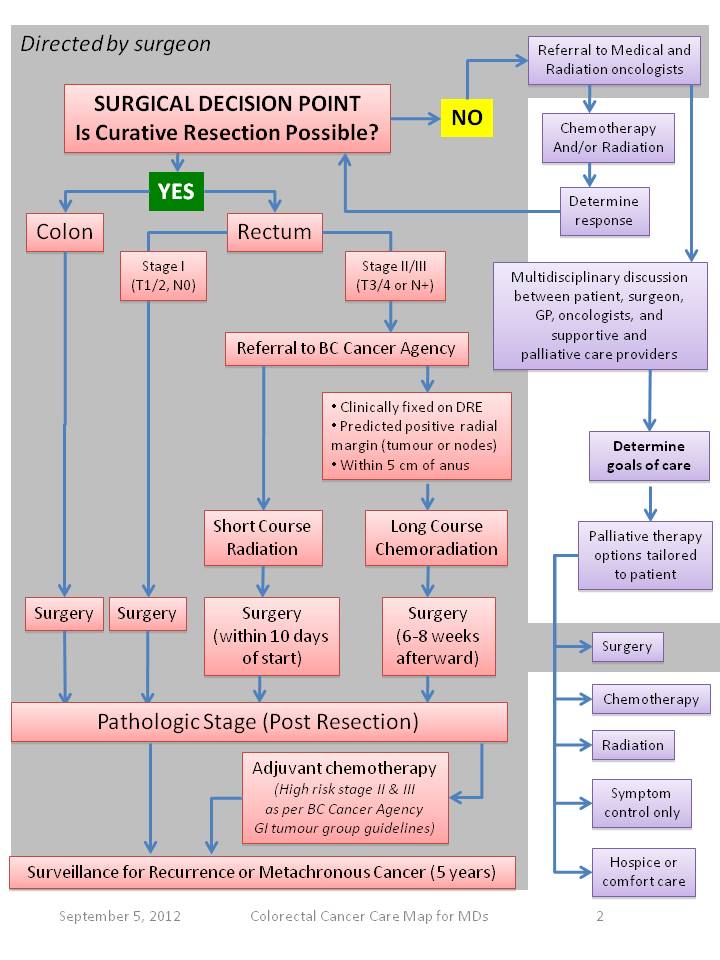
Please see the Colorectal Cancer Care Map for Physicians (below) developed by the BC Cancer Surgical Oncology Network and the accompanying text which is included in 8. Appendix.
- Neoadjuvant (preoperative) radiation therapy (with or without chemotherapy) for patients with clinical stage II or III rectal cancer is the preferred option as preoperative chemoradiation is less toxic and more effective than post-operative therapy. Referral for a Radiation/Medical Oncology consultation at the time of diagnosis is recommended.
- For patients with localized disease, the surgical standard of care is transabdominal resection with negative proximal, distal, and circumferential margins.
- For upper rectal tumours, a 5cm proximal and distal resection margin is standard (anterior resection), with en bloc lymphadenectomy (achieved by resecting the mesorectum to the distal rectal margin) and removal of all clinically suspicious lymph nodes outside the field of resection. Primary anastomosis is performed.
- For mid and lower rectal tumours, a total mesorectal excision (TME) with intact mesorectal envelope is performed, along with removal of all clinically suspicious lymph nodes. Primary anastomosis may be performed if a minimum 1-2 cm distal margin can be achieved (low anterior resection). Diverting loop ileostomy is recommended for low anastomoses, though is left to the discretion of the surgeon.
- For low rectal tumours where a 1-2 cm distal margin cannot be achieved, and abdominoperineal resection with permanent end colostomy is required
- Involved adjacent structures should be partially or completely resected where necessary to achieve a negative circumferential resection margin.
- Local, transanal resection may be considered in select circumstances where certain disease criteria are met or the patient is not a candidate for or refuses transabdominal resection (see below).
- Malignancy found during pathologic examination of an endoscopic polypectomy specimen can be considered definitive therapy only if the polyp can be completely assessed (removed in one piece), the tumour is well- or moderately-differentiated, there is no lymphovascular or perineural invasion, and the deep margin to malignant cells is greater than 3mm.
- In patients with obstructing or near-obstructing rectal cancer, a diverting loop colostomy may be performed to allow neoadjuvant radiation prior to definitive resection.
- For those with metastatic disease, resection of asymptomatic primary tumours is not routinely recommended, although retrospective evidence is conflicting with some studies demonstrating an improved survival associated with resection of the primary tumour. Palliative resection of the primary tumour, palliative (chemo)radiation or creation of a defunctioning loop colostomy may be done in patients with obstructive, hemorrhagic, or otherwise symptomatic rectal cancers. For selected patients with single organ metastases (stage M1a), resection of metastatic disease may be curative. Referral to BC Cancer for multi-disciplinary review is recommended.