Positron emission tomography (PET) imaging is a procedure that, when combined with computed tomography (CT), help physicians to more accurately diagnose and manage disease, especially cancer.
PET detects changes in cellular metabolism (how active a cell is), often indicating the presence of disease. CT detects changes in the physical size or shape of a lesion and shows exactly where in the body the lesion is located. By combining these two imaging technologies into a single scanner, we are now able to more accurately detect cancer and pinpoint its location in the body.
Together, PET and CT can be very helpful, for example, in the preoperative staging of some cancer types and in localizing suspected cancer recurrence when standard tests are inconclusive. This type of information can help physicians improve treatment planning for individual patients.
|

|
|
Normal PET Scan
|
Normal CT Scan
|
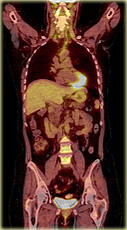
Fused PET/CT Scan
|
Active cells such as malignant cancer cells will use sugar as an energy source. Inactive cells such as benign cells and scar tissue (both noncancerous) will not use sugar as an energy source.
In PET, a special type of sugar is combined with a safe radioactive component to produce the radioactive tracer called FDG (Fluorodeoxyglucose). Once injected into a vein, the tracer, which emits signals detected by the scanner, will be absorbed by malignant cells but will not be absorbed by benign cells and scar tissue. This will indicate whether or not a lesion could be cancerous.
Combined with the localizing abilities of CT, this information can be used, for example, to show a surgeon the exact location of a malignant lesion that needs to be removed.
Upon arrival to the Molecular Imaging and Therapy department, you will be asked to complete a brief questionnaire. A technologist will take you to an examination room to explain the procedure and answer any questions you may have. You will then receive the tracer injection and be asked to relax in the private exam room for approximately 60 minutes to allow the tracer to circulate throughout your body. When this "uptake" period is complete, we will take you to the scan room to begin imaging.
You will lie on the imaging table which will slowly move you through the scanner while collecting data. For most procedures, you will be able to listen to music during the scan. The scan itself will last approximately 20 - 40 minutes depending on the type of scan ordered by your physician.
Once the scan has been completed and reviewed for technical quality, the appointment concludes and you will be free to leave. The entire procedure, from the time you arrive at BC Cancer until the time you leave, will last approximately 2 hours. A report will be sent to your physician once the scan has been read by a PET physician at BC Cancer.
A PET/CT scan is considered a diagnostic procedure similar to those done in Radiology and Nuclear Medicine. With over 2 million PET scans having been performed worldwide to date, there have been no reports of any adverse reaction to the tracer. Although there is a small amount of radiation exposure involved in your PET/CT scan, the exposure level is small and within the acceptable limits mandated by Health Canada for these types of procedures.
Also, tracers used in PET/CT have very short half-lives meaning they don't remain in your body very long. Twenty-four hours after your PET/CT scan, we would not be able to take any more images because the tracer will have completely left your body.
