Updated September 2013
Malignant pleural effusion (MPE) is a common clinical problem in the advanced stages of many cancers. The most common malignancies resulting in MPE are lung and breast cancer. For lung cancer patients, 45% will develop a MPE sometime during their illness, and 50% of advanced breast cancer patients will develop an effusion. It is associated with a poorer prognosis and the most common symptoms are dyspnoea and cough.
Treatment options depend on multiple factors including patient symptoms, performance status, prognosis and speed of reaccumulation of the pleural fluid. MPE is likely to reaccumulate in the majority of cases particularly if a patient is not able to be offered further systemic therapy to control disease.
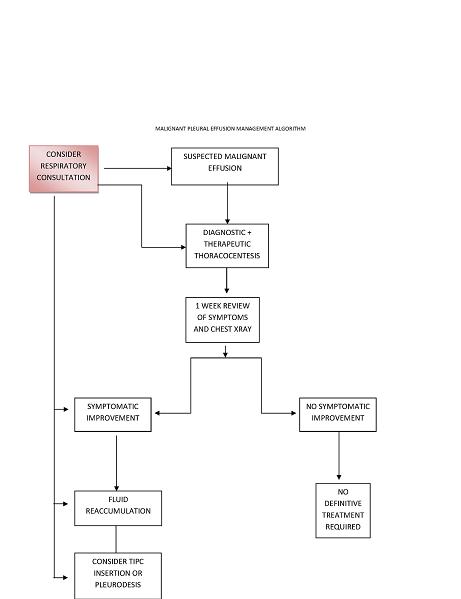
Patients with malignant pleural effusions may also develop complex pleural spaces rapidly with the formation of adhesions, loculations and trapped lung. Adequate assessment involves the use of imaging with chest x-ray, thoracic CT scan and thoracic ultrasound and the involvement of Respirologists/Thoracic Surgeons who are experienced in the management of MPE. Patients with suspected malignant effusions require early referral for the appropriate assessment due to the likelihood of reaccumulation and possible development of a complicated pleural space. (See below References for Management algorithm and Thoracocentesis checklist.)
Possible treatment options include:
- Intermittent thoracocentesis
- Talc pleurodesis – thoracoscopic or via chest tube
- Tunnelled indwelling pleural catheter eg PleurX system
1. Intermittent Thoracocentesis
An initial diagnostic and therapeutic thoracocentesis is indicated in the patient with a suspected MPE. It can be performed in the ambulatory setting under local anesthesia. Subsequent further use of repeated therapeutic thoracocentesis can be used on an intermittent basis for the rare patient who has a slowly accumulating effusion that only requires drainage every few months for symptom relief. It is also useful in the patient with a poor performance whose prognosis is < 4-6 weeks and the use of a more aggressive treatment option is not appropriate. It is not appropriate to use multiple repeated therapeutic thoracocenteses for symptom relief due to the risk of infection, empyema, pneumothorax and promotion of a complicated pleural space. The use of small pigtail catheters for prolonged drainage is discouraged due to frequent blockage within 72 hours and the promotion of loculations. If pigtail catheters are utilized, removal after 24 hours of fluid drainage is recommended.
2. Talc Pleurodesis
Talc pleurodesis can be performed via thoracoscopy under general anesthesia, pleuroscopy under local anesthesia and conscious sedation or via a chest tube with talc slurry. It requires inpatient hospital admission for a usual duration of 7 days. The patient must have a fully expandable lung for pleurodesis to be achieved and therefore, those with a trapped lung are excluded from this treatment option. Pleurodesis can be achieved in ~70% of patients without trapped lung but there is a risk of ARDS, infection, pneumonia and respiratory failure. Therefore, this option is usually limited to patients with limited comorbidities, good performance status and prognosis who are able to undergo the procedure and hospital admission.
3. Tunnelled Indwelling Pleural Catheters (TIPC)
The implementation of this technique for management of MPE has increased significantly in the last 5 years and it has largely replaced the use of talc pleurodesis for the majority of patients. Initial series reported its benefit in patients with poor performance status, but it has also been shown to be useful in patients with good performance status who may have been traditional candidates for pleurodesis. It remains the only treatment option for patients with trapped lung. In patients without trapped lung, spontaneous pleurodesis has been reported in 30-70% cases within 2-3 months.
Patient selection is important and evaluation with thoracic ultrasound necessary. Therefore, patients require evaluation by trained Respirologists/Thoracic surgeons with expertise in patient evaluation, TIPC insertion as well as longterm follow-up to manage any issues that may arise. The procedure is usually performed in the ambulatory setting under local anesthesia and light conscious sedation. The patient requires prior referral to the Palliative Care Benefits Schedule and the appropriate Community Nursing program at the time of the procedure. It can be inserted during chemotherapy or radiation therapy without increased risk of complications.
TIPC should not be inserted in patients with:
- Empyema
- Compromised skin at the site of the insertion due to malignancy, infection or radiation change
- Multi- loculated pleural space
- Anticoagulation, thrombocytopenia or bleeding diathesis
- Lack of available Community nursing services
- Prognosis < 4-6 weeks
- Inability to lie nearly flat for 30 minutes in lateral decubitus position
- No symptomatic improvement with previous thoracocentesis
References
Putnam J, Walsh G, Swisher S, Roth J, Suell D, Vaporciyan A, et al. Outpatient management of malignant pleural effusion by a chronic indwelling pleural catheter. Ann Thorac Surg, 2000;69:369-375.
Tremblay A, Michaud G. Single-center experience with 250 tunnelled pleural catheter insertions for malignant pleural effusion. Chest, 2006;129:362-368.
Tremblay A, Mason C, Michaud G. Use of tunneled catheters for malignant pleural effusions in patients fit for pleurodesis. Eur Respir, 2007;30:759-762.
Van Meter M, McKee K, Kohlwes J. Efficacy and safety of tunneled pleural catheters in adults with malignant pleural effusions: a systematic review. J Gen Intern Med, 2010;26:70-76.
Suzuki K, Servais E, Rizk N, Solomon S, Sima C, Park B, et al. Palliation and pleurodesis in malignant pleural effusion: the role for tunneled pleural catheters. J Thorac Oncol, 2011;6:762-767.
MacEachern P, Tremblay A. Pleural controversy: Pleurodesis versus indwelling pleural catheters for malignant effusions. Respirology, 2011;16:747-754.